What is Thalassemia?
Wednesday, July 20, 2016
What? Inherited blood disorder characterized by abnormal formation of hemoglobin (absent or decreased) and red blood cells in the body.
Why? Mutation in DNA of cells that make hemoglobin: Which? Alpha- and beta-thalassemia are the most common with different forms depending on type and number of mutations.
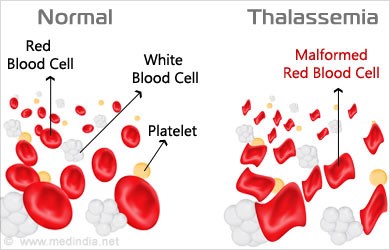
Hemoglobin production > Red Blood Cells destruction > oxygen to tissues > atigue and anemia
How common in UAE?
8.5% carriers of beta-thalassemia 49% carriers of alpha-thalassemia
Beta-thalassemia Inherited Pattern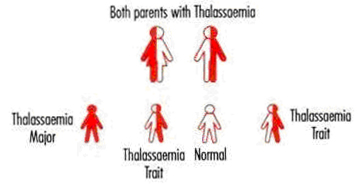
Where?
Alpha is common in:
African
Middle Eastern
East Indian
Chinese
Occasionally Mediterranean (Italian and Greek)
Beta is common in:
Mediterranean
Iranian
Gulf
African
Chinese
Southeast Asia
SYMPTOMS if carrier?
Asymptomatic or mild iron deficiency anemia
SYMPTOMS if affected?
- Fatigue
- Weakness
- Poor appetite
- Pale appearance
- Yellow discoloration of skin (jaundice)
- Slow growth
- Abdominal swelling
- Dark urine
- Enlarged spleen
- Bone deformities
- Heart problems
What is known in thalassemia?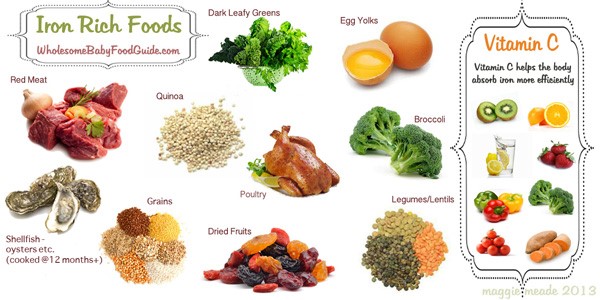
- Mild thalassemia may not need treatment, but the more severe form requires regular blood transfusions.
- Mildly increased energy expends. Hence, well-balanced and nutrient dense diet can help you feel better and boost your energy.
- If you are unlikely to obtain all your needs from diet alone consider taking multivitamin/mineral supplement.
- Iron intake should be monitored in case of overload.
- Vitamin D and zinc deficiencies are of particular concern and related to secondary health problems of thalassemia, such as iron deposition in certain organs, which will affect bone formation. Hence, consider 2000 IU/d of vitamin D and 20-90 mg/d of zinc in case of low bone mass.
- Folic acid deficiency is common; supplement may be recommended to make new red blood cells.
- No sufficient evidence suggests high dose of antioxidants from supplements will be beneficial.
- Protect yourself from infections through good hygiene, annual flu shots and vaccines (e.g. hepatitis B, pneumococcal).
Iron overload?
Too much iron from regular blood transfusions or increased absorption in the gut, will accumulate to toxic levels.
Low-iron diet:
- Limit high iron foods:
Meat iron: oyster, sardines, liver, beef, lamb and chicken.
Non-meat iron: beans, tofu, peanut butter, tofu, flour tortillas, cream of wheat fortified food items with iron and cereals. Also consider eliminating spinach, broccoli, leafy green vegetables prunes, dates and raisins.
*Absorption of iron into our body from non-meat sources is lower than that of meat sources.
- Iron-chelating agents may be prescribed by your doctor
Decrease iron absorption in your body:
- Avoid vitamin C rich foods (e.g. orange juice).
- Increase intake of dairy products, particularly calcium-rich foods: milk, yogurt, cheeseDrink tea or coffee with meals.
- Supplements without iron and vitamin C (e.g. Centrum Silver).
- Iron deposition in testis of young men and ovaries of young women can cause early menopause in women and require hormone replacement therapy (testosterone and estrogen) in both men and women.
What do we know about thalassemia and exercise?
- Exercise capacity is reduced due to anemia and iron-related cardiotoxicity (i.e. iron overload).
- Heart rate and cardiac output were reported to be abnormally high during exercise when having thalassemia.
- Aim for 150 min/week of moderate exercise and start progressively!
 By Ms. Ayla Coussa
By Ms. Ayla Coussa
Clinical Dietitian









